Type 2 Diabetes
Diabetes, defined as elevated blood sugar, is a disorder of metabolism, i.e., the way the body uses digested food for growth and energy. If not controlled, diabetes can be life threatening and associated with long-term complications that can affect every system and part of the body. Diabetes is classified into different types, based on various causes. Type 2 diabetes is by far the most common from of the disease, representing 80% to 90% of diabetes cases worldwide.
Type 2 Diabetes and Obesity
Type 2 diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage. It can affect pregnancy and cause birth defects, as well.
About 80 percent of persons with Type 2 diabetes are overweight.
Of those, some are severely or morbidly or obese. A standard way to define overweight, obesity, and morbid obesity is with the body mass index (BMI), a measure of body fat based on height and weight. The average BMI is 25. Morbid obesity is defined as:
- A BMI of 40.0 or higher is considered severely (or morbidly) obese
- A BMI of 35.0 or higher in the presence of at least one other significant co-morbidity (diabetes, coronary artery disease, hypertension, sleep apnea, or degenerative joint disease) is also classified as morbid obesity.
An individual can determine whether they are obese or morbidly obese using aBMI calculator.
Why Bariatric Surgery?
For most people who are simply overweight or obese, but not morbidly obese, diet and exercise are generally the best and safest way to reduce weight and health risks. The risks of bariatric surgery are thought to outweigh the risk of future medical problems and premature death.
However, for men who are more than 100 pounds overweight or women more than 80 pounds, bariatric or weight-loss surgery has been shown to be the most effective treatment. For a person who is morbidly obese, or obese with at least one co-morbidity such as Type 2 diabetes, there is significantly higher risk of worsening health problems or premature death so the risk of bariatric surgery is justified
Non-surgical treatments, such as diet modification, exercise programs, medications and social support programs have generally been ineffective in treating severe obesity, regardless of the approach used with rates of recurrence as high as 90%. Many can lose weight temporarily, but then regain it. There are currently no effective pharmacologic agents to treat obesity.
Because, severe obesity is a chronic condition that is difficult to treat through diet and exercise alone, bariatric or weight-loss surgery is an option for people who are severely obese and cannot lose weight by traditional means or who suffer from serious Type 2 diabetes or other obesity-related health problems.
Bariatric surgery is now accepted as the treatment of choice for producing significant and durable weight loss in morbidly obese patients. Bariatric surgery does this by restricting food intake and/or interrupting the digestive process to prevent the absorption of some calories and nutrients.
For severely obese patients with higher than normal blood sugar or pre-diabetic, bariatric surgery can reduce or eliminate the risk of developing Type 2 diabetes. For patients who already have Type 2 diabetes, the surgery can dramatically reduces its severity and, in some cases, cure the person of diabetes.
Glucose Metabolism and Diabetes
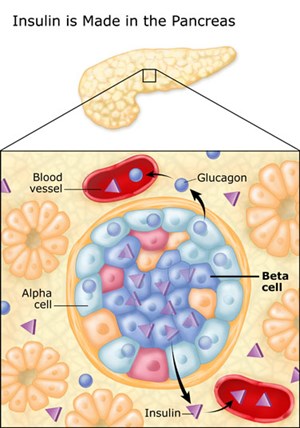
Most of the food people eat is broken down into glucose, the form of sugar in the blood. Glucose is the main source of fuel for the body. After digestion, glucose passes into the bloodstream, where it is used by cells for growth and energy. For glucose to get into cells, insulin must be present. Insulin is a hormone produced by the pancreas, a large gland behind the stomach.
|
|
| ImageCourtesy of UCSF Diabetes Education Online |
The pancreas is an organ about the size of a hand located in the abdomen in the vicinity of the stomach, intestines, and other organs. It lies behind the stomach and in front of the spine. The pancreas produce juices that help digest food and hormones such as insulin and glucagon that maintain optimal blood sugar levels and help the body to use and store energy from food.
Throughout the pancreas are clusters of cells called the islets of Langerhans. Islets are made up of several types of cells, including beta cells that make insulin. Insulin is a hormone that helps the body use glucose for energy.
Insulin and Type 2 Diabetes
Diabetes develops when the body doesn't make enough insulin, cannot use insulin properly, or both, causing glucose to build up in the blood. Diabetes is a serious disease, which, if not controlled, can be life threatening. It is often associated with long-term complications that can affect every system and part of the body. Diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage.
When a person eats, the pancreas automatically produces the right amount of insulin to move glucose from blood into the cells. In people with Type 2 diabetes, the cells do not respond appropriately to the insulin that is produced. Glucose builds up in the blood, overflows into the urine, and passes out of the body in the urine. Thus the body loses its main source of fuel even though the blood contains large amounts of glucose.
When type 2 diabetes is diagnosed, the pancreas is usually producing enough insulin, but for unknown reasons the body cannot use the insulin effectively, a condition called insulin resistance. After several years, insulin production decreases. The result is the same as for type 1 diabetes-glucose builds up in the blood and the body cannot make efficient use of its main source of fuel.
Who Develops Type 2 Diabetes
About 90 to 95 percent of people with diabetes have Type 2. The symptoms of type 2 diabetes develop gradually. Symptoms may include fatigue, frequent urination, increased thirst and hunger, weight loss, blurred vision, and slow healing of wounds or sores. Some people have no symptoms.
Type 2 diabetes is most often associated with older age, obesity, family history of diabetes, previous history of gestational diabetes, physical inactivity, and certain ethnicities. Type 2 diabetes is increasingly being diagnosed in children and adolescents, especially among African American, Mexican American, and Pacific Islander youth.
How is diabetes diagnosed?
The fasting blood glucose test is the preferred test for diagnosing diabetes in children and nonpregnant adults. The test is most reliable when done in the morning. However, a diagnosis of diabetes can be made based on any of the following test results, confirmed by retesting on a different day:
- A blood glucose level of 126 milli grams per deciliter (mg/dL) or higher after an 8-hour fast. This test is called the fasting blood glucose test.
- A blood glucose level of 200 mg/dL or higher 2 hours after drinking a beverage containing 75 grams of glucose dissolved in water. This test is called the oral glucose tolerance test (OGTT).
- A random-taken at any time of day-blood glucose level of 200 mg/dL or higher, along with the presence of diabetes symptoms.
Scope and impact of diabetes?
Diabetes is widely recognized as one of the leading causes of death and disability in the United States. In 2006, it was the seventh leading cause of death. However, diabetes is likely to be underreported as the underlying cause of death on death certificates. In 2004, among people ages 65 years or older, heart disease was noted on 68 percent of diabetes-related death certificates; stroke was noted on 16 percent of diabetes-related death certificates for the same age group.
Diabetes is associated with long-term complications that affect almost every part of the body. The disease often leads to blindness, heart and blood vessel disease, stroke, kidney failure, amputations, and nerve damage. Uncontrolled diabetes can complicate pregnancy, and birth defects are more common in babies born to women with diabetes.
In 2007, diabetes cost the United States $174 billion. Indirect costs, including disability payments, time lost from work, and reduced productivity, totaled $58 billion. Direct medical costs for diabetes care, including hospitalizations, medical care, and treatment supplies, totaled $116 billion.
How is diabetes managed?
Healthy eating, physical activity, and blood glucose testing are the basic management tools for type 2 diabetes. In addition, many people with type 2 diabetes require one or more diabetes medicines-pills, insulin, and other injectable medicine-to control their blood glucose levels.
Adults with diabetes are at high risk for cardiovascular disease (CVD). In fact, at least 65 percent of those with diabetes die from heart disease or stroke. Managing diabetes is more than keeping blood glucose levels under control-it is also important to manage blood pressure and cholesterol levels through healthy eating, physical activity, and the use of medications, if needed. By doing so, those with diabetes can lower their risk. Aspirin therapy, if recommended by a person's health care team, and smoking cessation can also help lower risk.
People with diabetes must take responsibility for their day-to-day care. Much of the daily care involves keeping blood glucose levels from going too low or too high. When blood glucose levels drop too low-a condition known as hypoglycemia-a person can become nervous, shaky, and confused. Judgment can be impaired, and if blood glucose falls too low, fainting can occur.